Ultrafiltration/Hemoconcentration
An often-overlooked and under-utilized method of blood management, providing a missing key in the quest for autologous blood conservation and salvaging for surgical patients
Ultrafiltration is a process of removing non-cellular water and low molecular weight solutes including cytokines, anaphylatoxins and platelet inhibitors from anticoagulated blood. This process has been available for over thirty years. Ultrafiltration maintains all the formed elements of whole blood such as red and white blood cells, platelets, clotting factors, plasma proteins, antibodies, albumin, vitamins, minerals, and most drugs or medications, all of which contribute to the stability, hemostasis and overall homeostasis of the surgical patient.
Ultrafiltration can be applied to anticoagulated blood that is either in the native circulation or in extracorporeal circuits, or blood that is collected and held in reservoirs for salvaging and eventual return to the patient, providing concentrated hyperoncotic autologous whole blood in a timely fashion.
Traditionally, the more modern methods of blood salvaging today involve direct infusion of diluted whole blood or the centrifugation of red cells or cell processors and salvage devices that wash and save red blood cells, i.e., "cell washers" or RBC-savers. These methods are efficient and readily acceptable in almost all surgical arenas, but are not without limitations.
Direct infusion of diluted whole blood produces hemodilution with crystalloid I.V. volume and lowers the viscosity and COP. Such blood contains activated cytokines and anaphylatoxins, which create abnormal volume kinetics and leads to organ edema and organ dysfunction. The kidneys are then stressed even more to overcome the oncotic challenge of diluted blood over an extended period of time (4–8+ hrs) to restore normovolemic homeostasis at a critical time for the patient, thus greatly increasing the risk of morbidity and mortality.
In contrast, RBC-savers are effective at removing water and concentrating blood by tightly packing cells in a centrifuge drawn from a reservoir. Subsequent washing removes cytokines, anaphylatoxins, anticoagulants and other waste substances that may have been collected in the reservoir suctioned from the surgical field.
The limitation is that cell savers also remove most of the other formed elements found in whole blood except red blood cells. With large volumes processed, this may lead to a coagulopathy, or worse, that of cell salvaged syndrome or DIC requiring blood product usage and other interventions to stabilize coagulation.
Ultrafiltration is not without its own limitations. Careful attention must be applied to the blood that is going to be hemoconcentrated, blood that it is anticoagulated and free of substances not intended for reinfusion.
The end product of hemoconcentration is hyperoncotic whole blood that increases the viscosity and COP, but is still anticoagulated and may need to be reversed with the use of protamine. With this in mind, ultrafiltration remains an untapped missing key that we can apply to better patient care with the patient’s best interest first and paramount.
At a time in society when a patient’s own blood is at a premium, ultrafiltration is rapidly gaining in popularity in the surgical arena. It provides a quick, easy, and efficient way to save more of the patient’s own blood and will help in the fight to reduce the use of allogeneic blood products with their associated costs, fears, and morbidity & mortality.
Ultrafiltration provides a viable alternative for blood salvaging and blood management in surgery, offering an efficient way to achieve hyperoncotic autologous whole blood for our patients and helping to stabilize the patients quickly. This comes at a time when globally we all need to re-evaluate the use of allogeneic transfusions and the consequences of doing so, and look for constructive, reliable and safe methods of reproducibly managing autologous blood, and avoid discarding viable and vital native cell fractions.
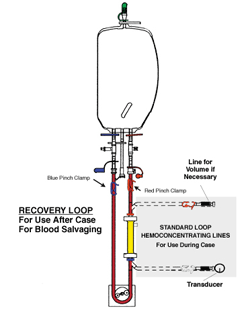
Presently, the only whole blood ultrafiltration device in clinical use
is the Hemobag®
Hemoconcentrator Reference
Also see Ultrafiltration Literature